Electronic Remittance Advice (ERA/EOB, EDI 835)
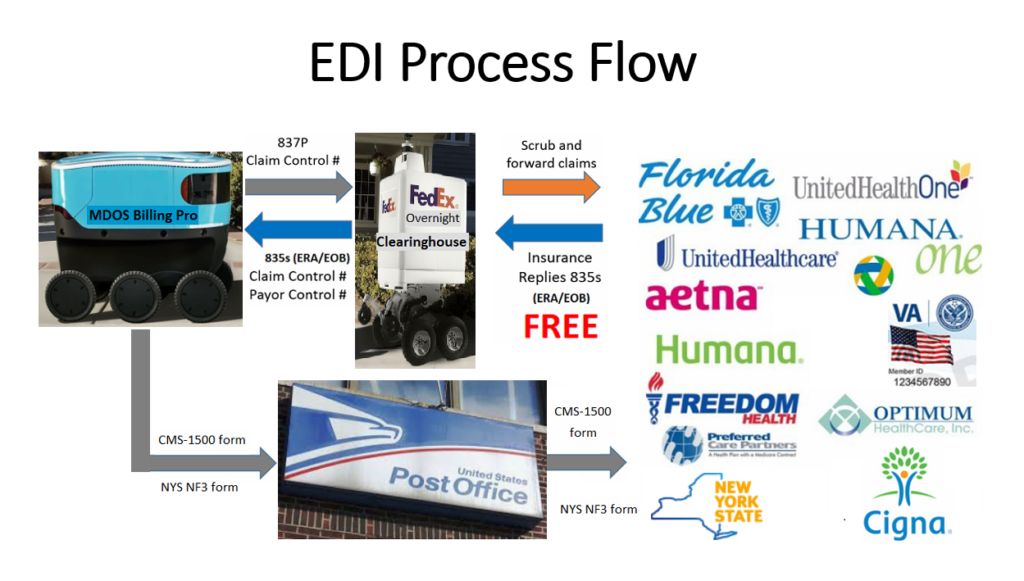
EDI Process Flow
After verifying that no information is missing in the claim, MDOS Billing Pro software generates the EDI 837P claim file. The EDI 837P claim file is then uploaded to a clearinghouse, which will be further validated by the clearinghouse before forwarding to a payer. The claim payment information is created after the claim is received and adjudicated by a payer. The Electronic Remittance Advice (ERA), or EDI 835, is the electronic transaction that provides claim payment information.
If the claim submitting provider has ERA enrollment with the payer, the payer will send the payment ERA files to the clearinghouse designated by the provider. Office Ally Electronic Remittance / ERA / 835 Enrollment Forms can be found out at Payer ERA Enrollment Forms (A-Z). Electronic Remittance Advice (ERA) is a free service provided by a payer. All a provider needs to do is to have ERA enrollment with a payer.
The provider can FTP or download the payment ERA files from the clearinghouse. These ERA files are used by practices, facilities, and billing companies to auto-post claim payments into their systems. The benefits of auto-posting claim payments are:
- Eliminate manual keying; save time and effort
- Reduce posting errors
- Increase efficiency and save money
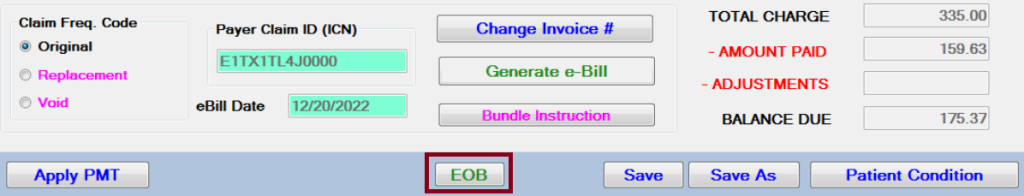
Electronic EOB
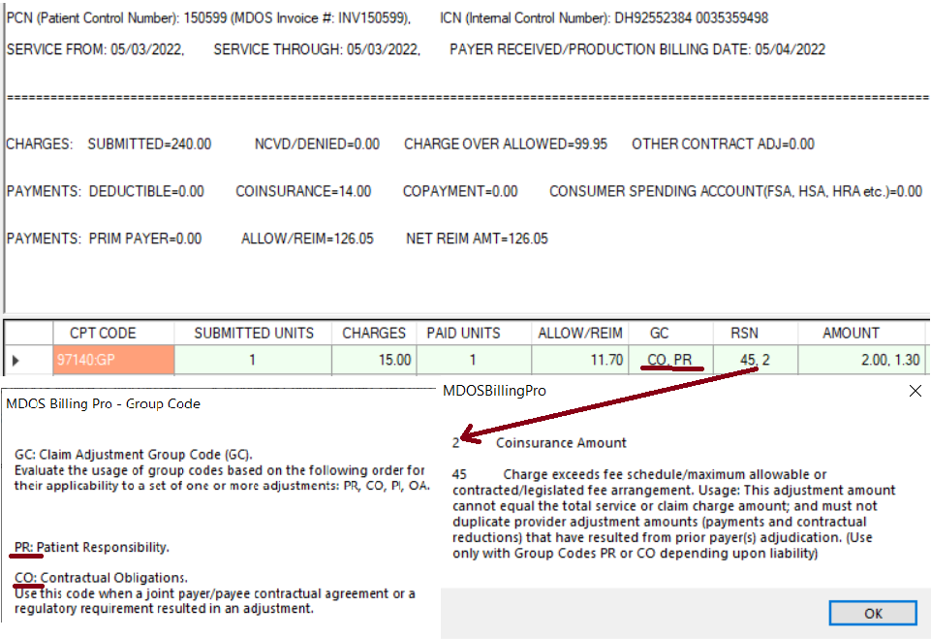
Downloaded ERA 835 files from a clearinghouse are imported and auto-posted into the MDOS Billing Pro system. The electronic EOB is added to the claim and becomes part of the claim. Unlike in a clearinghouse where the users have to search for the claim EOBs, the MDOS users can view insurance payments for each CPT code and how the payer pays each CPT code in the electronic EOB (Explanation Of Benefits) conveniently in the claim.
The following information is available in the auto-posted 835 Electronic Remittance Advice – ERA file in the MDOS Billing Pro system:
- Claim Invoice Number
- Service Date
- Check Number
- Remittance Date
- Patient Insurance Member ID
- Patient Account Number
- Provider Name and NPI
- Payer’s Claim Control Number
- Claim Charge Amount
- Claim Charge Over Allowed Amount
- Claim Deductible Amount
- Claim Coinsurance Amount
- Claim Copay Amount
- Consumer Spending Amount (FSA, HAS, HRA, etc.)
- Primary Payer Paid Amount
- Claim Allowed Amount
- Claim Net Reimbursement Amount
- Procedure Code
- Procedure Units
- Procedure Charges
- Procedure Paid Units
- Procedure Allowed Amount
- Procedure Group Code
- Procedure Charge Allocation Reason Code
- Procedure Payment for Each Reason
- Procedure Remittance Advice Remark Code
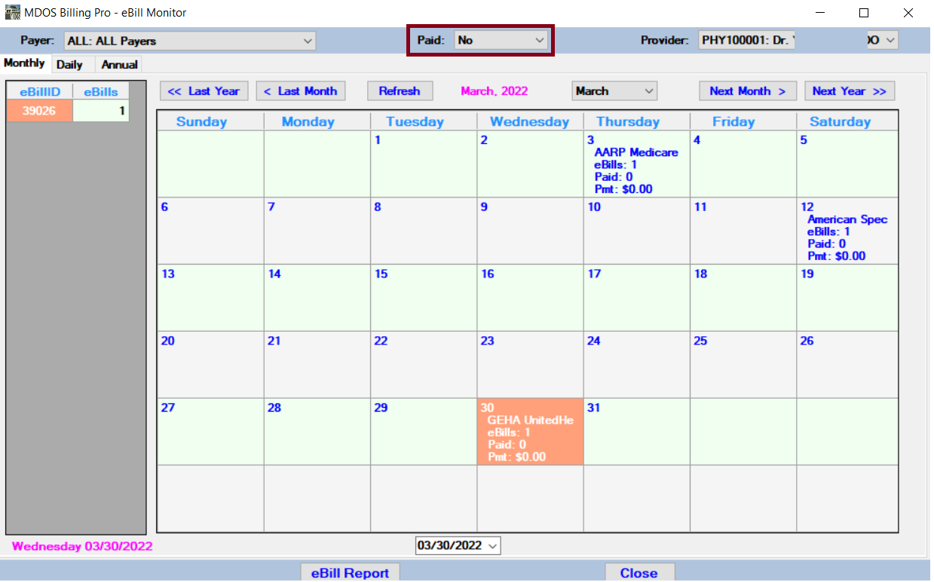
Track Electronic Remittance Advice (ERA) insurance payments
We use the auto-posted ERA insurance payments to track claims and can concentrate on the few unpaid claims. ERA insurance payment tracking saves a lot of effort for the providers and enables them to work on unpaid claims promptly and get them paid eventually. The claim status for the unpaid claims can be checked out electronically with MDOS Billing Pro EDI 276/277: Claim Status Inquiry and Response to save time and money.
ERA Deductible, Copayment, and Coinsurance
Besides listing the insurance payment in the invoice report, the Deductible, Copayment, and Coinsurance from the ERA are also listed in the invoice report as the post-ERA insurance benefits verification.
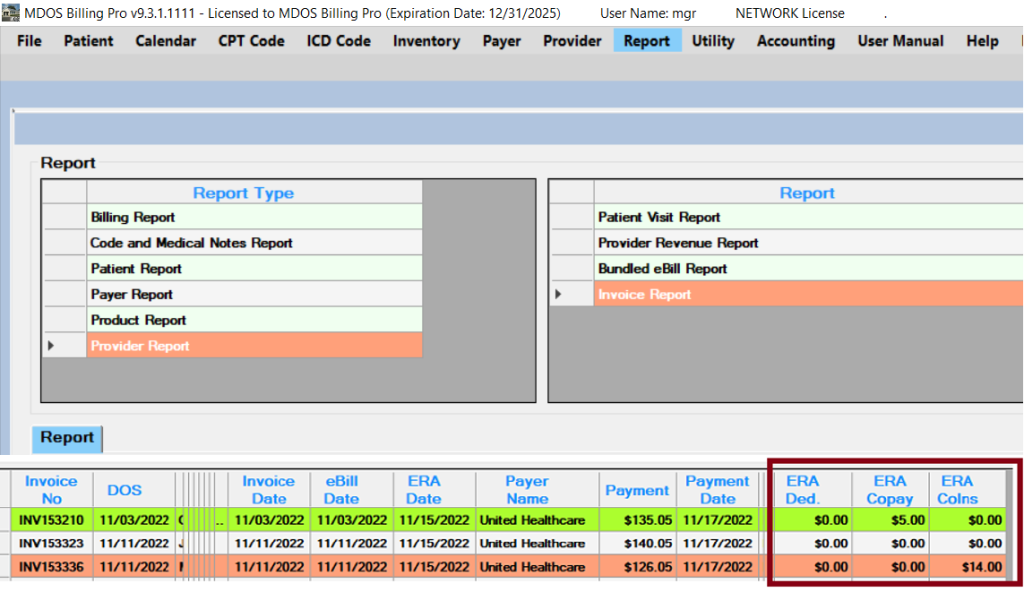
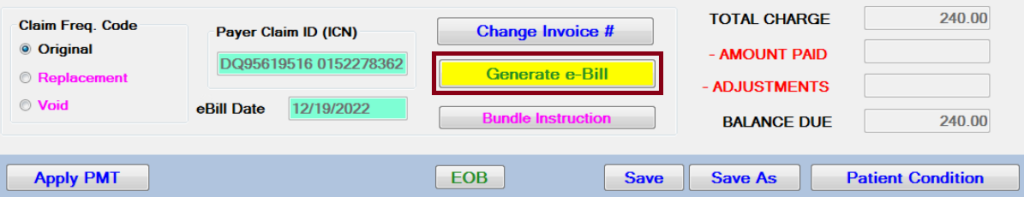
The Generate e-Bill button is highlighted when the patient is in the deductible phase.