Electronic Claim Submission (EDI 837P)
Electronic Claim vs. Manual Claim
An “electronic claim” is a paperless patient claim form generated by practice management software that is transmitted electronically over the internet to a healthcare payer for processing and payment, while a “manual claim” is a paper claim form that refers to either the Centers for Medicare & Medicaid Services CMS-1500 form (formerly HCFA-1500) or a Uniform Billing UB-04 form. These both are typically sent to the payer through the mail and require postage. In electronic claim submission, the claims are filed electronically which automatically reduces the chances of claim errors and improves accuracy, so the claims are processed more quickly.
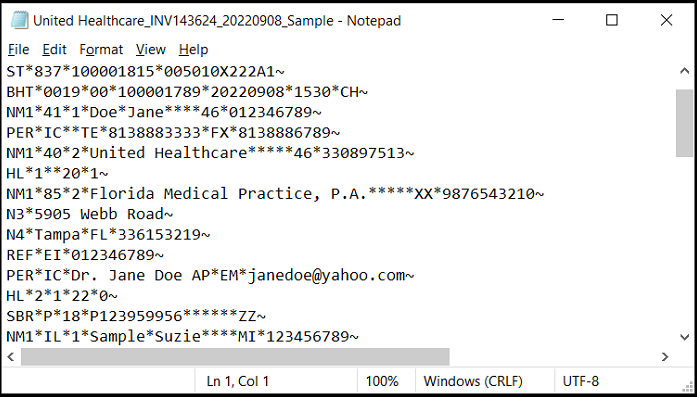
A sample of the electronic claim is presented below.
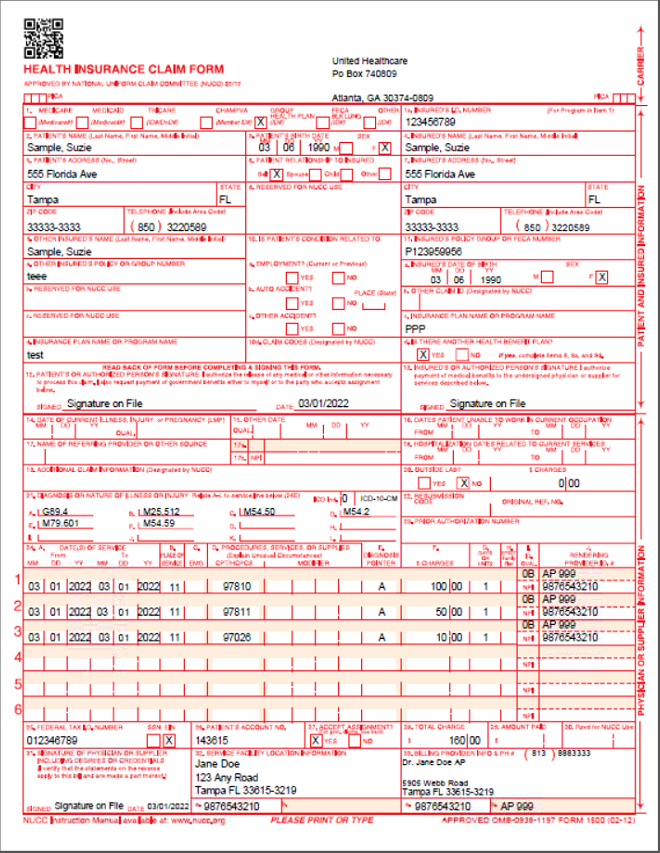
A sample of the paper manual claim is shown below.
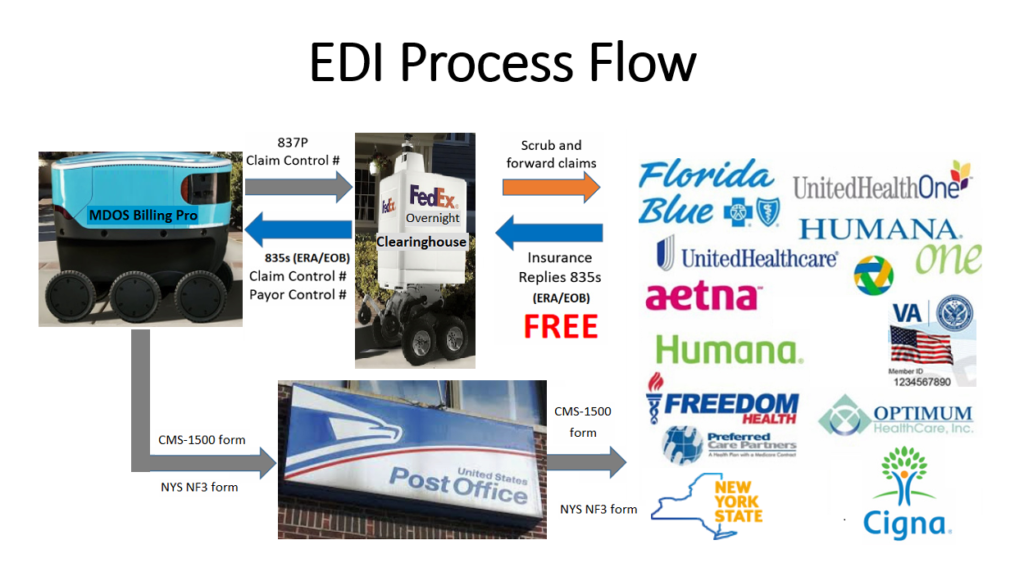
EDI Process Flow
After verifying that both patient information and insurance payer information are available and complete, an electronic claim, the EDI 837P file, is generated. The EDI 837P claim file is then uploaded to a clearinghouse, which will be further validated by the clearinghouse before forwarding to a payer. The claim payment information is created after the claim is received and adjudicated by a payer. The Electronic Remittance Advice (ERA), or EDI 835 can be used to view and auto-post the claim payment information. The EDI 276/277: Claim Status Inquiry and Response can be used to check out the claim status electronically.
The benefit of electronic claim submissions is saving time and cost. It reduces the amount of time as well as the need for resources to devote to a manual administrative function. Instead, this time can be better spent with patients or focused on other practice efficiencies.
Electronic claims submission can:
- Pre-audit claim fields automatically for potential errors before submission to a payer
- Detect claim issues and offer online claim resolution before processing by a payer
- Submit claims almost instantaneously or overnight to a payer
- Reduce postage, supplies, and mailing expenditures
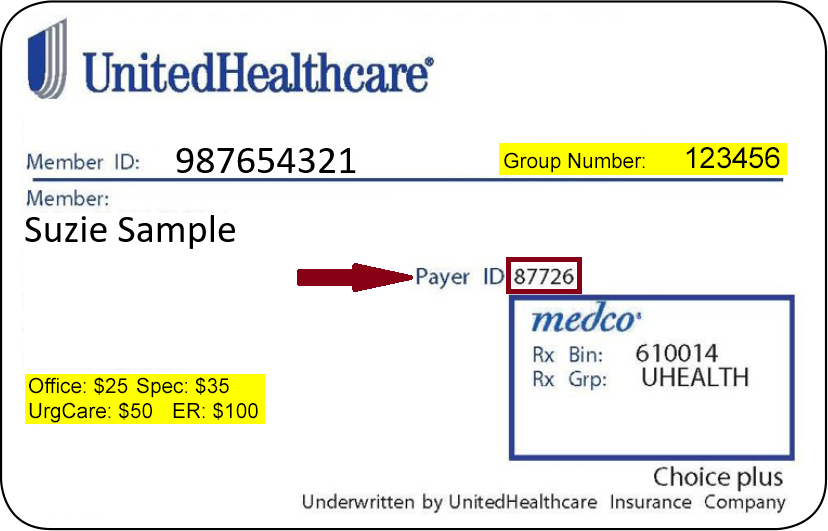
Payer ID
We need to put the address on the envelope for a letter so that it can be delivered by the post office to the recipient. The same thing applies to electronic claim submissions. The Payer ID is used to route electronic claims to the appropriate payer. Like zip code, a Payer ID has a length of five, but it can be both numbers and letters. The member’s ID card will indicate the Payer ID to use for claims submissions as shown below.
If the Payer ID cannot be found on the member’s ID card, we need to look up the Payer ID on the clearinghouse payer list.
Electronic Claim Submission with MDOS Billing Pro Software
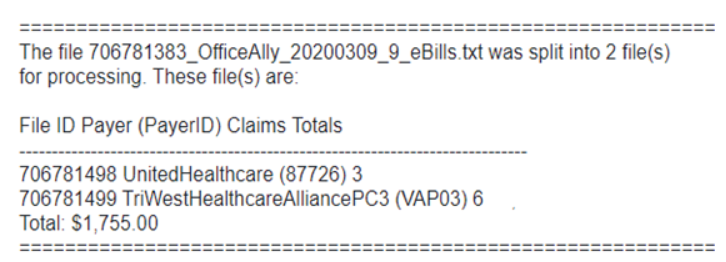
MDOS Billing Pro is Windows-based desktop software and runs on Windows 7, 8, 10, or 11 for small businesses that can have total control of their medical data and send electronic medical claims. MDOS Billing Pro allows physicians, practitioners, and other medical providers to electronically submit claims to a clearinghouse with 837P files generated in our system. The generated 837P claim files are then combined and bundled into one file, uploaded to a clearinghouse, then routed to various payers electronically based on the claims Payer ID, as shown below.
Initial visit claims are generated easily from the customized pre-built CPT Claim templates. Subsequent new claims are generated conveniently by changing the previous claim’s service date.
All the 95 thousand ICD-10 Codes are loaded into our system and updated annually for free. We provide billing support to claims rejected/denied by the payers. MDOS Billing Pro is not just billing software, but a billing solution.
Paper Form CMS-1500 Manual Claim Submission with MDOS Billing Pro
Occasionally some claims have to be sent traditionally in paper form. MDOS Billing Pro allows you to print your CMS-1500 red form on white paper as shown above.
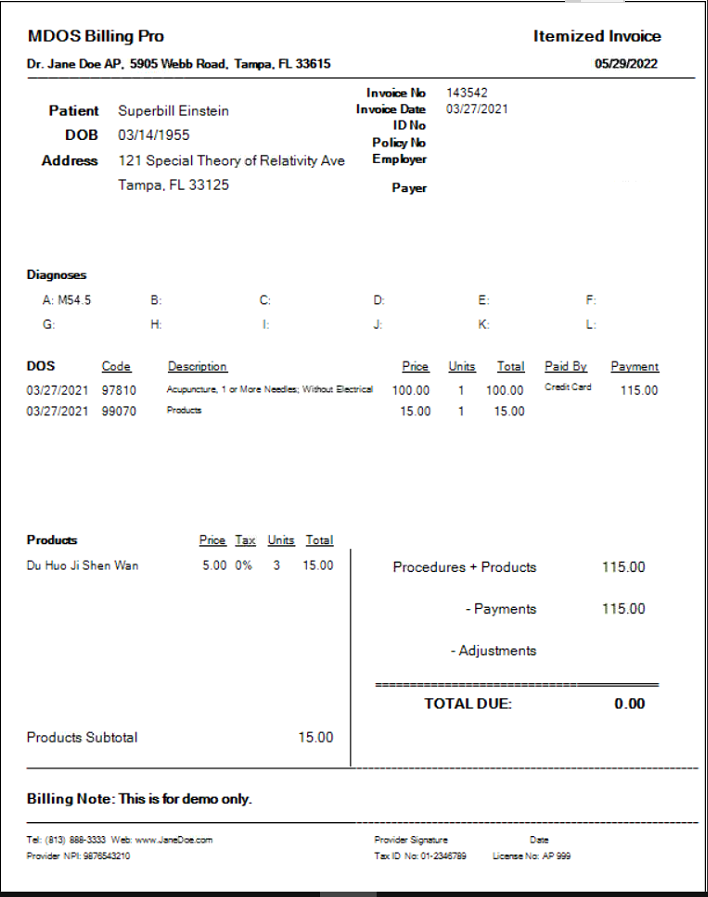
Superbill and Inventory
MDOS Billing Pro also allows to creation and printing of Superbills. The users don’t have to use two systems: One for insurance billing patients and the other for cash patients. MDOS Superbills also work with the inventory system seamlessly and can check out products with a barcode scanner or product name.